Associação Portuguesa de Investigação em Cancro
Os linfócitos intra-tumorais estromais e a expressão de PDL1 estão associados a formas agressivas de carcinoma da mama
Os linfócitos intra-tumorais estromais e a expressão de PDL1 estão associados a formas agressivas de carcinoma da mama
Recentemente foi publicado no Journal of Clinical Pathology um trabalho desenvolvido pelo i3S/Ipatimup sobre o papel dos linfócitos intra-tumorais estromais (LITs) e da expressão do PDL1 em carcinomas da mama.
Usando duas séries independentes de carcinoma da mama (uma delas incluindo carcinomas in situ), os autores foram capazes de relacionar os LITs e a expressão de PDL1 a carcinomas da mama de grau histológico elevado (grau 3) e ao subtipo molecular triplo-negativo, características associadas a pior prognóstico. Verificaram ainda a presença pela primeira vez da expressão de PDL1 nas células de carcinoma in situ e de uma estreita relação com marcadores de células estaminais. Por fim, observaram ainda que determinados carcinomas da mama associados a expressão de PDL1 apresentavam pior prognóstico, podendo eventualmente ser alvo de terapêuticas dirigidas contra esta molécula.
Autores e afiliações:
António Polónia 1,2,3,4, Regina Pinto 1,2,3, Jorge F. Cameselle-Teijeiro 5, Fernando C. Schmitt 1,2,3,4,6, Joana Paredes 1,2,4
1 Epithelial Interactions in Cancer (EPIC), i3S – Instituto de Investigação e Inovação em Saúde, University of Porto, Porto, Portugal;
2 Ipatimup, Institute of Molecular Pathology and Immunology of the University of Porto, Porto, Portugal;
3 Department of Pathology, Ipatimup Diagnostics, Ipatimup, University of Porto, Porto, Portugal;
4 FMUP, Faculty of Medicine, University of Porto, Porto, Portugal;
5 Complexo Hospitalar Universitario de Vigo (CHUVI), Vigo, Spain;
6 Laboratoire National de Santé, Dudelange,Luxembourg
Abstract:
AIM: The present work aims to evaluate the presence of stromal tumour-infiltrating lymphocytes (TILs) and programmed cell death-ligand 1 (PDL1) expression in breast carcinomas and their correlation with available clinicopathological features.
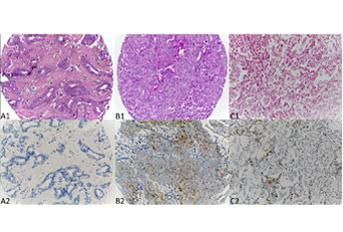
METHODS: Two independent series of invasive breast cancer (IBC), one including ductal carcinoma in situ (DCIS) pair-matched cases, were selected, and quantification of TILs was accomplished in each case. Immunohistochemistry was also performed to evaluate the expression of PDL1.
RESULTS: In both cohorts evaluated, increased stromal TILs and PDL1 expression were present in about 10% of IBCs, being significantly associated with each other and both with grade 3 and triple-negative subtype. We observed a similar distribution of stromal TILs and PDL1 expression between DCIS and IBC. Finally, we observed that increased stromal TILs and PDL1 expression were significantly associated with cancer stem cell (CSC) markers, basal cell markers and vimentin expression. Interestingly, in IBC cases with vimentin expression, increased stromal TILs, as well as decreased PDL1 expression, disclosed a better clinical outcome, independently of the main classical BC prognostic factors.
CONCLUSIONS: We have confirmed the association of stromal TILs and PDL1 expression with aggressive forms of BC and that both are already found in in situ stages. We also showed that stromal TILs and PDL1 expression are associated with clinical outcome in cases enriched for a mesenchymal immunophenotype. We describe for the first time a close relationship between CSC markers and PDL1 expression.
Revista: Journal of Clinical Pathology
Link: http://jcp.bmj.com/content/early/2017/04/03/jclinpath-2016-203990.long




