Associação Portuguesa de Investigação em Cancro
Adherence, risk perception, and attitudes towards colorectal cancer screening: A road to individualized screening?
Adherence, risk perception, and attitudes towards colorectal cancer screening: A road to individualized screening?
O cancro colorretal é uma das principais causas de morte por cancro a nível mundial. Em Portugal, o rastreio populacional por pesquisa de sangue oculto nas fezes (PSOF) foi implementado na região Norte em 2018. Um estudo recente avaliou a intenção da população em participar no rastreio, as suas preferências quanto ao método utilizado e as principais barreiras identificadas. A maioria dos participantes (95%) demonstrou intenção de aderir ao rastreio, sobretudo quando compreendia o seu propósito. No entanto, muitos desconheciam os sintomas e fatores de risco associados ao cancro colorrectal. A PSOF foi o método preferido por 25% dos participantes que nunca tinham sido rastreados, sendo vista como menos invasiva do que a colonoscopia. A colonoscopia, por sua vez, mostrou ser mais aceite entre quem já tinha sido submetido a esse exame. Estes resultados sugerem que uma informação clara sobre o rastreio e a oferta de alternativas, como a colonoscopia para quem recusa a PSOF, podem aumentar a participação nos programas de rastreio.
João Carlos Silva a , b , c , ∗,Mário Dinis-Ribeiro b , c , Fernando Tavares d ,Diogo Libânio b , c
a Gastroenterology Department, Unidade Local de Saúde Gaia e Espinho (ULSGE), Vila Nova de Gaia, Portugal
b MEDCIDS, Faculty of Medicine, University of Porto, Portugal
c Gastroenterology Department, RISE@CI-IPOP (Health Research Network), Portuguese Oncology Institute of Porto (IPO Porto) & Porto Comprehensive Cancer Centre (Porto.CCC), Porto, Portugal d Studies and Planning Department, Northern Portugal Regional Health Administration (ARSN), Porto, Portugal
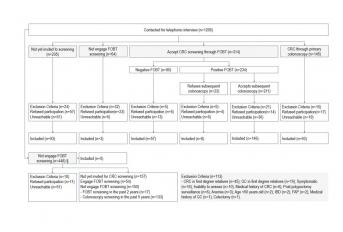
Background & Aims: Colorectal cancer (CRC) ranks second globally in cancer-related deaths and there is ongoing debate on the best populational screening strategy. This study aimed to evaluate individuals’ intention to adhere to CRC screening, screening method preference, and barriers to screening. Methods: Cross-sectional study conducted in northern Portugal, where a populational fecal occult blood test (FOBT) program is implemented. The validated PERCEPT-PREVENT tool was administered across 3 groups: a) not yet invited to screening b) accepted FOBT screening, and c) primary colonoscopy screening. Results: A total of 397 participants completed the PERCEPT-PREVENT questionnaire and were compared by screening status. Intention to adhere was reported at a high rate (95%; n = 354) and was positively influenced by knowledge of the screening rationale (OR 8.96, 95% CI 3.61-22.25). Most were unaware of symptoms (64 %; n = 253), risk factors (68 %; n = 271), and associated screening procedure risks (58 %; n = 230). Lower barrier scores for FOBT (7 ± 3) compared to colonoscopy (10 ± 3) were ob- observed for screening naïve respondents ( p < 0.001). Previous FOBT screening led to a lower preference for colonoscopy (previous FOBT screening 56 % vs not yet invited to screening 75 % vs previous primary colonoscopy 90 %; p < 0.001). Discussion: A greater understanding of the screening rationale enhances adherence. FOBT was highly accepted among never-screened participants. Colonoscopy should be offered to FOBT decliners, as personalized screening approaches could improve participation rates.
Digestive and Liver diseases
https://www.dldjournalonline.com/article/S1590-8658(24)01119-8/fulltext




