Associação Portuguesa de Investigação em Cancro
A aneuploidia identifica subgrupos de doentes com evolução clínica desfavorável no cancro da mama de grau 1 e grau 2
A aneuploidia identifica subgrupos de doentes com evolução clínica desfavorável no cancro da mama de grau 1 e grau 2
Neste estudo, que incluiu 684 doentes com carcinoma invasivo da mama e “fcancro da mama, António Evaristo Pintoollow-up” de longo prazo, observámos que aquelas que apresentaram tumores aneuploides com grau 1 e grau 2 de diferenciação, quando comparados com os diplóides, tiveram pior prognóstico, tanto na série total como no cancro precoce da mama (estádios I/IIA da doença). Este achado tem implicações terapêuticas, pois estas doentes são potenciais candidatas a terapia adjuvante adaptada ao risco.
Autores e Afiliações:
António E. Pinto1, Teresa Pereira1, Giovani L. Silva2, Saudade André1
1Serviço de Anatomia Patológica, Instituto Português de Oncologia de Lisboa Francisco Gentil, E.P.E., 1099-023 Lisboa, Portugal.
2Centro de Estatística e Aplicações e Departamento de Matemática do Instituto Superior Técnico, Universidade de Lisboa, 1049-001 Lisboa, Portugal.
Abstract:
Objective: Histological grade is a well-established prognostic/predictive factor in breast cancer. However, mainly within intermediate categories, patients may have unpredictable outcome. We hypothesised whether ploidy status can distinguish different prognostic groups among breast cancer patients with similar tumour grade.
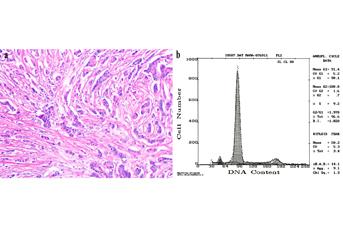
Material and methods: The study involved 684 patients with invasive breast carcinoma, and median follow-up of 134.5 months. Pathological staging was evaluated according to WHO classification. Tumour differentiation was assessed using the Nottingham grading system. Ploidy was determined prospectively by DNA flow cytometry. Disease-free survival (DFS) and overall survival (OS) were estimated by the Kaplan-Meier method.
Results: There were 179 (26.2%) deaths and 239 (33.3%) disease recurrences. For grading, tumours were classified as follows: 163 (23.8%) G1, 356 (52.1%) G2 and 165 (24.1%) G3, while 389 (56.9%) tumours presented aneuploidy. Ploidy and grading are strongly associated (P<0.001). Patients with aneuploid G2 tumours showed worse DFS (P=0.001) and OS (P<0.001), as well as those with aneuploid G1 tumours in relation to OS (P=0.013). When a subset analysis was performed in early breast cancer patients (n=451) with Stage I/IIA of disease, it remained the same significant associations of aneuploid G1 (to OS) and G2 tumours (to DFS and OS) with unfavourable prognosis.
Conclusions: Aneuploidy identifies subsets of breast cancer patients with G1 and G2 tumours who showed poor clinical outcome. The finding has therapeutic implications, as these patients are potential candidates to risk-adapted adjuvant therapy.
Revista: The Breast




