Associação Portuguesa de Investigação em Cancro
Influência dos macrófagos na resposta dos tumores da bexiga à terapêutica com BCG
Influência dos macrófagos na resposta dos tumores da bexiga à terapêutica com BCG
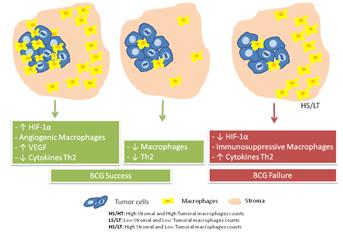
O carcinoma urotelial da bexiga tem elevada relevância em termos de perda da qualidade de vida e gastos em saúde. A terapêutica intravesical adjuvante com Bacillus Calmette-Guérin (BCG) veio melhorar a sobrevivência livre de doença, embora apresente uma taxa de recidiva de 30% e elevada morbilidade. A identificação de biomarcadores preditivos da recidiva/progressão, reveste-se assim de significativa relevância para a optimização terapêutica e com implicações no prognóstico. Embora existam evidências sobre os mecanismos envolvidos na acção anti-neoplásica da BCG, permanecem por clarificar os mecanismos responsáveis pela resistência ao tratamento. Estudos demonstraram que o BCG promove um ambiente inflamatório tipo Th1, o qual parece ser essencial para o sucesso da terapêutica. Níveis baixos de citocinas como interleucina-2 (IL-2), IL-8, IL-12, IL-18 e TNF-α e níveis elevados de citocinas do tipo Th2 (IL-10) parecem estar associados à falha da imunoterapia com BCG. A presença de macrófagos associados ao tumor (TAMs), em tumores removidos antes desta terapia, revelou ser um dos biomarcadores com resultados mais consistentes na literatura. Assim, o principal objectivo deste trabalho foi esclarecer a influência dos TAMs, em particular do subtipo M2, em áreas do estroma e do tumor, no contexto da resposta à terapia com BCG. Foi demonstrado que doentes com elevadas contagens de macrófagos CD163+, predominantemente localizados no estroma (contagens elevadas no estroma e baixas contagens na área tumoral) apresentam um risco acrescido de recidiva. Observamos também que estes macrófagos localizam-se em áreas com baixa expressão de HIF-1α, levantando a hipótese de que estes macrófagos poderão apresentar um fenótipo imunossupressor produzindo citocinas do tipo Th-2 que poderão inibir a resposta Th-1 necessária para a ação anti-tumoral desta terapêutica. Este trabalho vem reforçar o papel do microambiente tumoral na modelação de respostas às terapêuticas anti-tumorais.
Luís Lima 1,2,3,4 and Daniela Oliveira 1; Ana Tavares 1,5; Teresina Amaro 6; Ricardo Cruz 7; Maria J. Oliveira 8,9,10; José A. Ferreira 1,11 and Lúcio Santos 1,12,13.
1 Experimental Pathology and Therapeutics Group, Portuguese Institute of Oncology, Porto, Portugal
2 ICBAS, Abel Salazar Biomedical Sciences Institute, University of Porto, Porto, Portugal
3 Núcleo de Investigação em Farmácia - Centro de Investigação em Saúde e Ambiente (CISA), School of Allied Health Sciences – Polytechnic Institute of Oporto, Porto, Portugal
4 LPCC, Research Department-Portuguese League Against Cancer (NRNorte), Portugal
5 Department of Pathology, Portuguese Institute of Oncology, Porto, Portugal
6 Department of Anatomic Pathology, Hospital Pedro Hispano, Matosinhos, Portugal
7 Department of Urology, Portuguese Institute of Oncology, Porto, Portugal
8 INEB - Institute of Biomedical Engineering, Porto University
9 Department of Pathology e Oncology, Faculty of Medicine, Porto University
10 Department of Biology, Faculty of Sciences, Porto University
11 QOPNA, Mass Spectrometry Center of the University of Aveiro, Campus de Santiago, Aveiro, Portugal
12 Health Faculty of University Fernando Pessoa, Porto, Portugal
13 Department of Surgical Oncology, Portuguese Institute of Oncology, Porto, Portugal
OBJECTIVE: Bacillus Calmette-Guérin (BCG) immunotherapy is the gold standard treatment for superficial bladder tumors with intermediate/high risk of recurrence or progression. However, approximately 30% of patients fail to respond to the treatment. Effective BCG therapy needs precise activation of the type 1 helper cells immune pathway. Tumor-associated macrophages (TAMs) often assume an immunoregulatory M2 phenotype and may directly interfere with the BCG-induced antitumor immune response. Thus, we aim to clarify the influence of TAMs, in particular of the M2 phenotype in stroma and tumor areas, in BCG treatment outcome. PATIENTS AND METHODS: The study included 99 patients with bladder cancer treated with BCG. Tumors resected before treatment were evaluated using immunohistochemistry for CD68 and CD163 antigens, which identify a lineage macrophage marker and a M2-polarized specific cell surface receptor, respectively. CD68+ and CD163+ macrophages were evaluated within the stroma and tumor areas, and high density of infiltrating cells spots were selected for counting. Hypoxia, an event known to modulate macrophage phenotype, was also assessed through hypoxia induced factor (HIF)-1α expression. RESULTS: Patients in whom BCG failed had high stroma-predominant CD163+ macrophage counts (high stroma but low tumor CD163+ macrophages counts) when compared with the ones with a successful treatment (71% vs. 47%, P = 0.017). Furthermore, patients presenting this phenotype showed decreased recurrence-free survival (log rank, P = 0.008) and a clear 2-fold increased risk of BCG treatment failure was observed in univariate analysis (hazard ratio = 2.343; 95% CI: 1.197-4.587; P = 0.013). Even when adjusted for potential confounders, such as age and therapeutic scheme, multivariate analysis revealed 2.6-fold increased risk of recurrence (hazard ratio = 2.627; 95% CI: 1.340-5.150; P = 0.005). High stroma-predominant CD163+ macrophage counts were also associated with low expression of HIF-1α in tumor areas, whereas high counts of CD163+ in the tumor presented high expression of HIF-1α in tumor nests. CONCLUSIONS: TAMs evaluation using CD163 is a good indicator of BCG treatment failure. Moreover, elevated infiltration of CD163+ macrophages, predominantly in stroma areas but not in the tumor, may be a useful indicator of BCG treatment outcome, possibly owing to its immunosuppressive phenotype.
Revista:
Urologic Oncology: Seminars and Original Investigations
http://www.urologiconcology.org/article/S1078-1439(13)00454-7/abstract




