Associação Portuguesa de Investigação em Cancro
Compliance to radiation therapy of head and neck cancer patients and impact on treatment outcome
Compliance to radiation therapy of head and neck cancer patients and impact on treatment outcome
A study performed by Aveiro University and the School of Allied Health Technologies (IPP), in collaboration with the Portuguese Institute of Oncology of Coimbra (IPOCFG), within the scope of the research project RESPONSE quantified patient compliance to radiation therapy and the clinical benefits obtained in patients with head and neck tumours to the clinical protocol adopted by IPOCFG since 2006.
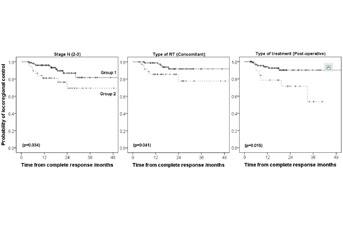
This study showed that patients that received radiation therapy as planned had a probability of tumour control 10-19% higher compared to patients that interrupted the treatment. These differences were statistically significant for the subgroup of patients with advanced tumours (stage N2-3), patients undergoing concomitant radiochemotherapy and post-operative patients. The major cause for interrupting radiation therapy was the severity of side-effects and intercurrent disease. Preventing measures that minimize treatment breaks are thus fundamental.
Authors and Afiliations:
BC Ferreira1,2, P Sa-Couto3, MC Lopes4, L Khouri5
1I3N Departamento de Física, Universidade, Aveiro
2 Escola Superior de Tecnologia de Saúde do Porto – Instituto Politécnico do Porto, Porto
3 Departamento de Matemática, Universidade de Aveiro, Aveiro
4 Serviço de Física Médica, Instituto Português Oncologia do Porto Francisco Gentil, Coimbra
5 Serviço de Radioterapia, Instituto Português Oncologia do Porto Francisco Gentil, Coimbra
Abstract:
Aims: Evaluate head and neck (HNC) cancer patient’s compliance to the planned radiation therapy (RT) using the department policy established in 2005 at IPOCFG. Estimate the impact in treatment outcome due to failure in receiving RT as prescribed.
Material and Methods: 359 HN cancer patients irradiated from 2007-2013 were included in this study. Patient cohort was divided into Group 1: patients receiving RT as prescribed and Group 2: patients that interrupted or suspended RT. Group Tox is the subgroup of patients that interrupted RT due toxicity or intercurrent disease. Number and causes for treatment interruptions were assessed. The cumulative incidence of locoregional control (LRC), disease free survival (DFS) and overall survival for Group 1 and 2 was determined. Cox regression was performed to investigate potential hazard factors and logistic regression was made to determine risk factors related to treatment interruptions.
Results: Major causes for treatment interruptions were toxicity plus intercurrent disease (41.7%) and public holidays (30.1%). 10.3% of the patients interrupted 3-9 days. Significant differences in survival distributions of LRC between Group 1 and 2, of up to 19%, were found for the subgroup of patients with N2-3 tumours, for post-operative RT and for concomitant RT. Treatment breaks larger than two days had an almost four-fold increased risk of poorer LRC and DFS.
Conclusions: Twin accelerators and treating on public holidays are effective measures minimizing RT breaks. For HNC, patient compliance is mostly limited by RT side-effects. Efforts to maintain RT biological effective dose in HNC must be always undertaken.
Journal: Clinical and Translational Oncology
Link: http://link.springer.com/article/10.1007/s12094-015-1417-5




